New findings in the mechanism of weight loss promote the improvement of obesity-related diseases
Obesity is a global, multifactorial disease defined as abnormal or excessive fat accumulation that presents a risk to health. Obesity is associated with several comorbidities, such as cardiovascular diseases (CVDs), metabolic syndrome, type 2 diabetes mellitus (T2DM) and cancer. Because of their increasing prevalence, significant impacts on health and medical costs, obesity with its comorbidities has become a public health concern. Traditionally, the cause of obesity is considered an imbalance between caloric intake and energy expended. Research has shown that a weight loss between 5% and 10% is enough to induce clinically relevant improvements in health risk factors such as raised blood glucose and other biomarkers related to augmented risk of CVD. Recently, a number of studies on the mechanism of weight loss have been reported, which may provide help for improving obesity-related diseases.
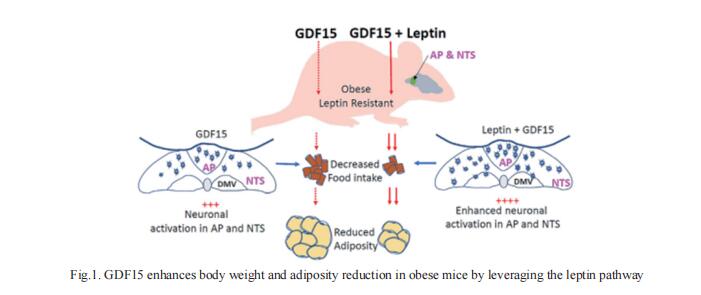
1. GDF15 enhances body weight and adiposity reduction in obese mice by leveraging the leptin pathway
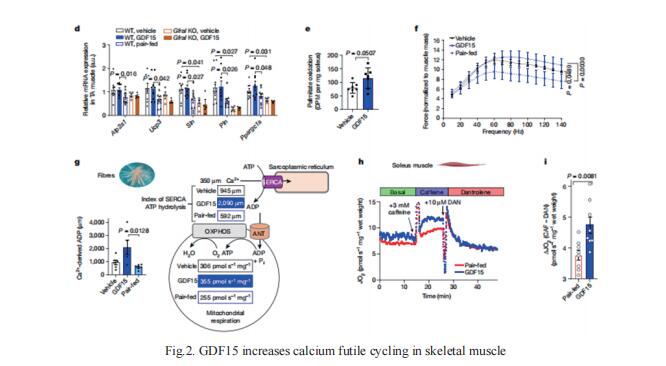
Growth differentiating factor 15 (GDF15) regulates its anorexic effects through the hindbrain area postrema (AP) and nucleus of the solitary tract (NTS) neurons where its receptor, glial-derived neurotrophic factor receptor alpha-like (GFRAL), is expressed. The actions of GDF15 may interact with other appetite regulators elevated in obesity, such as leptin. Samuel N. Breit, St Vincent’s Centre for Applied Medical Research, St Vincent’s Hospital, Sydney, Australia, and his team reported that in mice with high-fat-diet-induced obesity (HFD), the combined infusion of GDF15 and leptin causes significantly greater weight and adiposity loss than either treatment alone (Fig.1), indicating potentiation between GDF15 and leptin[1]. Furthermore, obese, leptin-deficient ob/ob mice are less responsive to GDF15, as are normal mice treated with a competitive leptin antagonist. GDF15 and leptin induce more hindbrain neuronal activation in HFD mice than either treatment alone does. They reported extensive connections between GFRAL- and LepR-expressing neurons and find LepR knockdown in the NTS to reduce the GDF15-mediated activation of AP neurons. Overall, these findings suggest that leptin signaling pathways in the hindbrain increase GDF15’s metabolic actions.
2. GDF15 promotes weight loss by enhancing energy expenditure in muscle
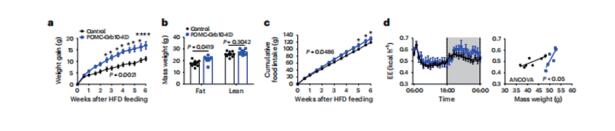
Caloric restriction that promotes weight loss is an effective strategy for treating non-alcoholic fatty liver disease and improving insulin sensitivity in people with type 2 diabetes. Despite its effectiveness, in most individuals, weight loss is usually not maintained partly due to physiological adaptations that suppress energy expenditure, a process known as adaptive thermogenesis, the mechanistic underpinnings of which are unclear. Treatment of rodents fed a high-fat diet with recombinant GDF15 reduces obesity and improves glycaemic control through GFRAL-dependent suppression of food intake. Gregory R. Steinberg, Centre for Metabolism, Obesity and Diabetes Research, McMaster University, Canada, and his team found that, in addition to suppressing appetite, GDF15 counteracts compensatory reductions in energy expenditure, eliciting greater weight loss and reductions in non-alcoholic fatty liver disease (NAFLD) compared to caloric restriction alone[2]. This effect of GDF15 to maintain energy expenditure during calorie restriction requires a GFRAL-β-adrenergicdependent signalling axis that increases fatty acid oxidation and calcium futile cycling in the skeletal muscle of mice (Fig.2). These data indicate that therapeutic targeting of the GDF15-GFRAL pathway may be useful for maintaining energy expenditure in skeletal muscle during caloric restriction.
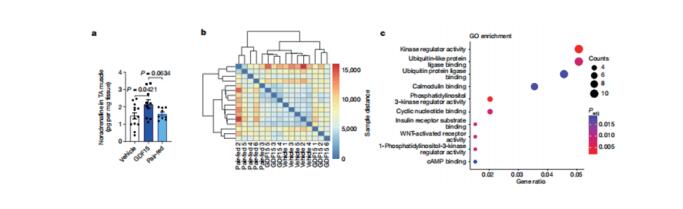
3. Hypothalamic Grb10 enhances leptin signalling and promotes weight loss
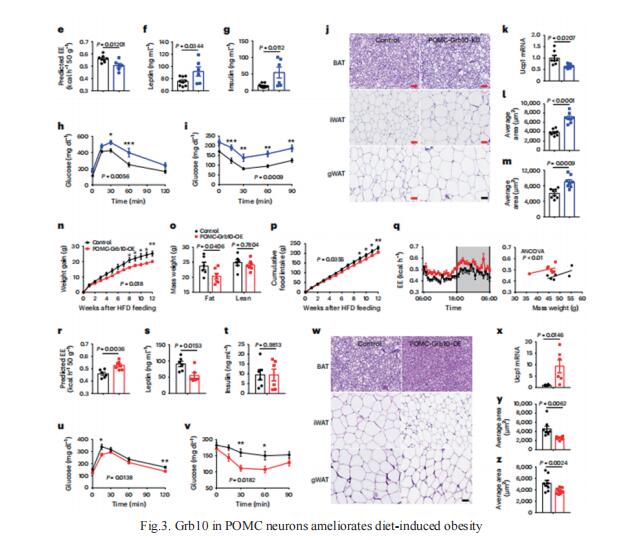
Leptin acts on hypothalamic neurons expressing agouti-related protein (AgRP) or pro-opiomelanocortin (POMC) to suppress appetite and increase energy expenditure, but the intracellular mechanisms that modulate central leptin signalling are not fully understood. Feng Liu, National Clinical Research Center for Metabolic Diseases, Metabolic Syndrome Research Center, Key Laboratory of Diabetes Immunology, Ministry of Education, Department of Metabolism and Endocrinology, The Second Xiangya Hospital of Central South University, China, and his team showed that growth factor receptor-bound protein10 (Grb10), an adaptor protein that binds to the insulin receptor and negatively regulates its signalling pathway, can interact with the leptin receptor and enhance leptin signalling[3]. Ablation of Grb10 in AgRP neurons promotes weight gain, while overexpression of Grb10 in AgRP neurons reduces body weight in male and female mice. In parallel, deletion or overexpression of Grb10 in POMC neurons exacerbates or attenuates diet-induced obesity, respectively (Fig.3). Consistent with its role in leptin signalling, Grb10 in AgRP and POMC neurons enhances the anorexic and weight-reducing actions of leptin. Grb10 also exaggerates the inhibitory effects of leptin on AgRP neurons via ATP-sensitive potassium channel-mediated currents while facilitating the excitatory drive of leptin on POMC neurons through transient receptor potential channels. The study identifies Grb10 as a potent leptin sensitizer that contributes to the maintenance of energy homeostasis by enhancing the response of AgRP and POMC neurons to leptin.
References
[1]Breit SN, Manandhar R, Zhang HP, Lee-Ng M, Brown DA, Tsai VW. GDF15 enhances body weight and adiposity reduction in obese mice by leveraging the leptin pathway. Cell Metab. 2023;S1550-4131(23)00219-X. (IF=29.0)
[2]Wang D, Townsend LK, DesOrmeaux GJ, et al. GDF15 promotes weight loss by enhancing energy expenditure in muscle. Nature. 2023;619(7968):143-150. (IF=64.8)
[3]Liu H, He Y, Bai J, et al. Hypothalamic Grb10 enhances leptin signalling and promotes weight loss. Nat Metab. 2023;5(1):147-164. (IF=20.8)
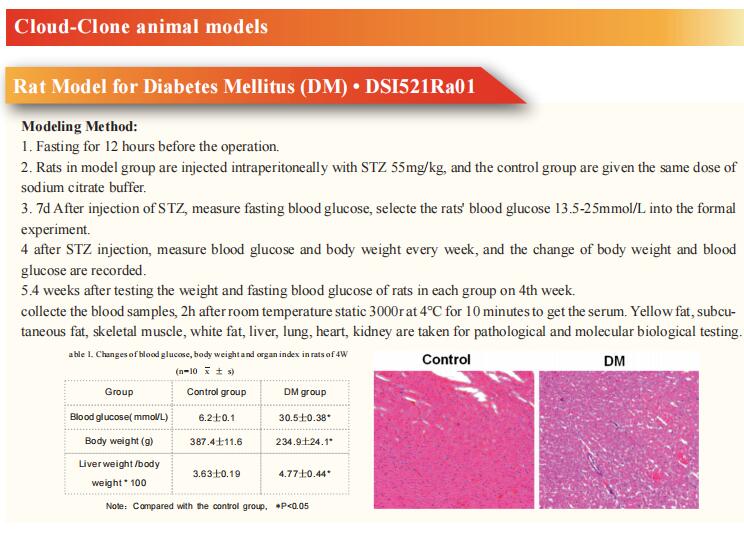
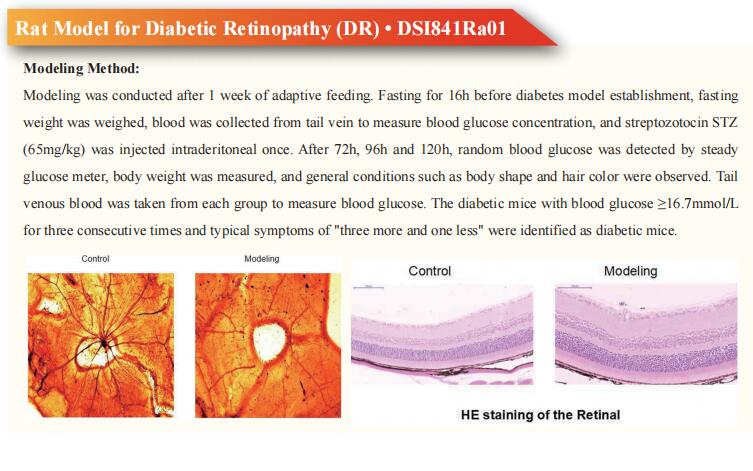
Cloud-Clone can not only provide a variety of animal models of obesity related diseases, including diabetes, hyperglycemia, cardiovascular diseases, non-alcoholic fatty liver and other common diseases. We also have various metabolic disorder detection indicators and the aforementioned GDF15, GFRα, LepR, AgRP, POMC, and Grb10 related products, which can help the majority of scientific researchers to carry out relevant research on the treatment of obesity-related diseases.